What is polycystic ovary syndrome (PCOS)?
Polycystic ovary syndrome (say "pah-lee-SIS-tik OH-vuh-ree SIN-drohm") is a problem in which a woman’s hormones are out of balance. It can cause problems with your periods and make it difficult to get pregnant. PCOS may also cause unwanted changes in the way you look. If it is not treated, over time it can lead to serious health problems, such as diabetes and heart disease.
Polycystic ovary syndrome (or PCOS) is common, affecting as many as 1 out of 15 women. Often the symptoms begin in the teen years. Treatment can help control the symptoms and prevent long-term problems.
What are hormones, and what happens in PCOS?
Hormones are chemical messengers that trigger many different processes, including growth and energy production. Often, the job of one hormone is to signal the release of another hormone.
For reasons that are not well understood, in PCOS the hormones get out of balance. One hormone change triggers another, which changes another. For example:
The sex hormones get out of balance. Normally, the ovaries make a tiny amount of male sex hormones (androgens). In PCOS, they start making slightly more androgens. This may cause you to stop ovulating, get acne, and grow extra facial and body hair.
The body may have a problem using insulin, called insulin resistance. When the body doesn't use insulin well, blood sugar levels go up. Over time, this increases your chance of getting diabetes.
What are the symptoms?
Symptoms tend to be mild at first. You may have only a few symptoms or a lot of them. The most common symptoms are:
- Acne.
- Weight gain and trouble losing weight.
- Extra hair on the face and body. Often women get thicker and darker facial hair and more hair on the chest, belly, and back.
- Thinning hair on the scalp.
- Irregular periods. Often women with PCOS have fewer than nine periods a year. Some women have no periods. Others have very heavy bleeding.
- Fertility problems. Many women who have PCOS have trouble getting pregnant (infertility).
- Depression.
Most women with PCOS grow many small cysts on their ovaries. That is why it is called polycystic ovary syndrome. The cysts are not harmful but lead to hormone imbalances.
What causes PCOS?
The symptoms of PCOS are caused by changes in hormone levels. There may be one or more causes for the hormone level changes.
PCOS seems to run in families, so your chance of having it is higher if other women in your family have PCOS, irregular periods, or diabetes. PCOS can be passed down from either your mother's or father's side.
How is PCOS diagnosed?
To diagnose PCOS, the doctor will:
Ask questions about your past health, symptoms, and menstrual cycles.
Do a physical exam to look for signs of PCOS, such as extra body hair and high blood pressure. The doctor will also check your height and weight to see if you have a healthy body mass index (BMI).
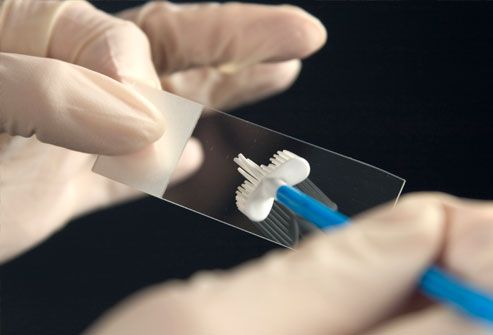
Do a number of lab tests to check your blood sugar, insulin, and other hormone levels. Hormone tests can help rule out thyroid or other gland problems that could cause similar symptoms.
You may also have a pelvic ultrasound to look for cysts on your ovaries. Your doctor may be able to tell you that you have PCOS without an ultrasound, but this test will help him or her rule out other problems.
How is it treated?
Regular exercise, healthy foods, and weight control are key treatments for PCOS. Medicines to balance hormones may also be used. Getting treatment can reduce unpleasant symptoms and help prevent long-term health problems.

The first step in managing PCOS is to get regular exercise and eat heart-healthy foods. This can help lower blood pressure and cholesterol and reduce the risk of diabetes and heart disease. It can also help you lose weight if you need to.
Try to fit in moderate activity and/or vigorous activity on a regular basis. Walking is a great exercise that most people can do.
Eat a heart-healthy diet. In general, this diet has lots of vegetables, fruits, nuts, beans, and whole grains. It also limits foods that are high in saturated fat, such as meats, cheeses, and fried foods. If you have blood sugar problems, try to eat about the same amount of carbohydrate at each meal. A registered dietitian can help you make a meal plan.
Most women who have PCOS can benefit from losing weight. Even losing 10lb may help get your hormones in balance and regulate your menstrual cycle. PCOS can make it hard to lose weight, so work with your doctor to make a plan that can help you succeed.
If you smoke, consider quitting. Women who smoke have higher androgen levels that may contribute to PCOS symptoms.1Smoking also increases the risk for heart disease.
A doctor may also prescribe medicines, such as:
Birth control pills. They can help your periods be regular and can reduce symptoms such as excess facial hair and acne. An androgen-lowering medicine, spironolactone, may be used with birth control pills to help reduce symptoms even more. These medicines are not used if you are trying to get pregnant.
A diabetes medicine called metformin. It can help restore regular menstrual cycles and fertility.
Fertility medicines, if you are trying to get pregnant.
It is important to see your doctor for follow-up to make sure treatment is working and to adjust it if needed. You may also need regular tests to check for diabetes, high blood pressure, and other possible problems.
It may take a while for treatments to help with symptoms such as facial hair or acne. In the meantime:
Over-the-counter or prescription acne medicines may help with skin problems.
Waxing, tweezing, and shaving are easy ways to get rid of unwanted hair. Electrolysis or laser treatments can permanently remove the hair but are more expensive. Your doctor can also prescribe a skin cream that slows hair growth for as long as you use it regularly.
It can be hard to deal with having PCOS. If you are feeling sad or depressed, it may help to talk to a counselor or to other women who have PCOS. Ask your doctor about local support groups, or look for an online group. It can make a big difference to know that you are not alone.